Understanding Healthcare Job Types: Staff vs. Per Diem vs. Travel
The benefits and drawbacks to consider when deciding which type of healthcare employment is right for you
Choosing a career path in healthcare means more than just selecting a job; it involves a deeper understanding of the field. Jobs in healthcare offer more than just a choice of workplace, they are your working lifestyle. Whether you prefer the stability of a staff job, the flexibility of per diem work, or the adventure of travel assignments, there’s a path that fits your goals and where you want life to take you. Because in healthcare, it’s not just about where and when you work, but how and why you work.
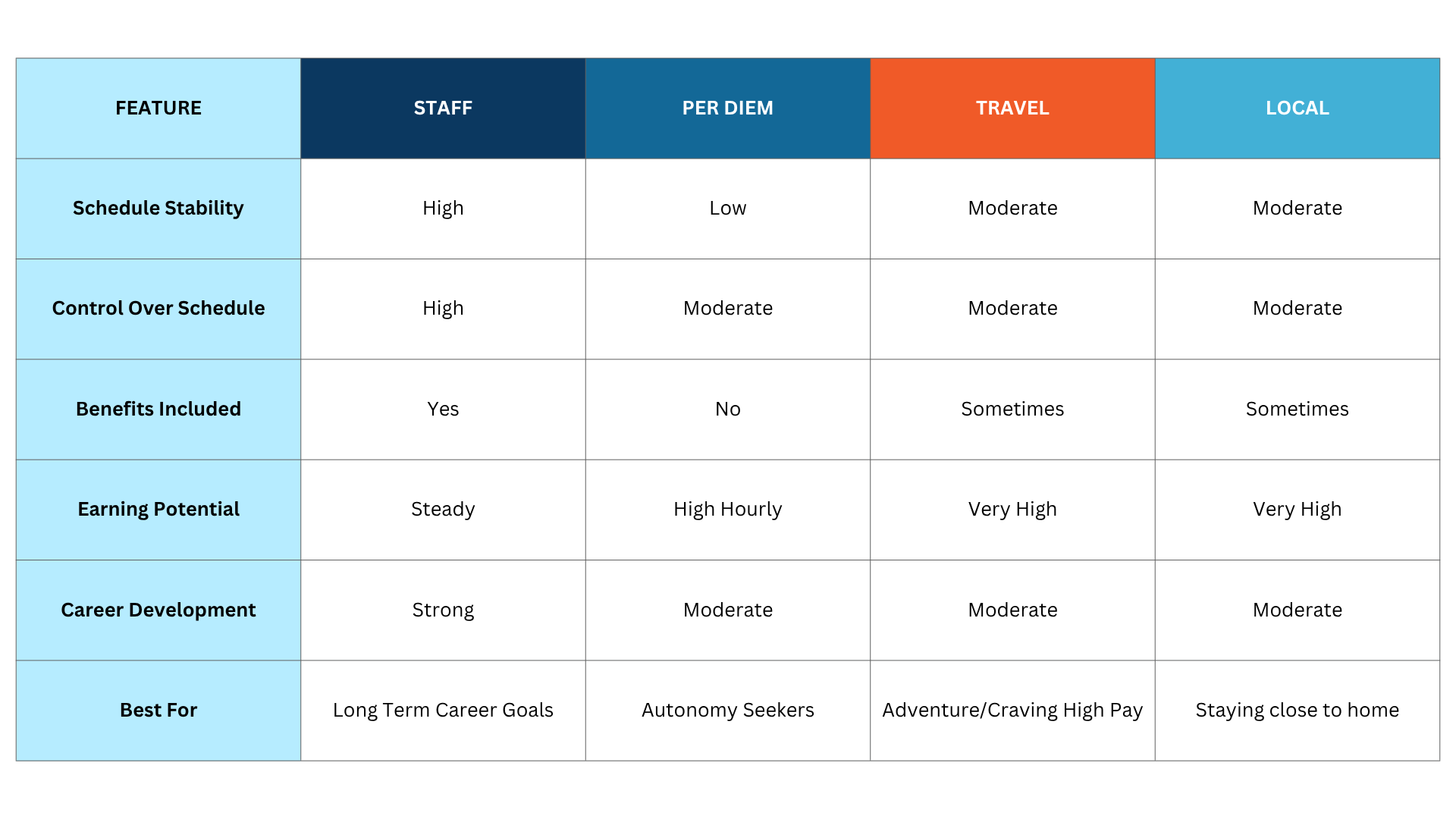
Each pathway – travel, per diem, and staff — has its own set of pros, cons, and unique features. There’s a difference between these positions, allowing you to assess the lifestyle, income potential, and career potential of each. As with any job in any industry, you want to make sure you’re selecting the best type of job that suits your short-term needs and long-term career goals. That’s the great thing about a healthcare career: there are options for everyone. Whether you want stability, flexibility, or travel, there’s a role at a facility that you’ll love.
Staff Positions: Permanent (Perm)/full time
Staff positions are permanent roles where healthcare professionals, such as nurses, CT technologists, sonographers, anesthesia assistants, and doctors, among others, are directly employed by a hospital, clinic, long-term care facility, short-term care facility, or doctor’s office. These roles are usually full-time but can also be part-time, with a steady weekly schedule.
Perm Advantages:
- Job stability – predictable hours and long-term employment. You can plan days off on a consistent schedule each week. Depending on the job setting, you may have nights and weekends off.
- Full benefits – health insurance, paid time off, retirement plans, and possible tuition reimbursement for continuing education.
- Team building – opportunities to be part of a consistent team to build strong relationships, enhance knowledge-sharing, and form long-term co-worker relationships.
- Career advancement and growth — access to internal promotions, training programs, and professional development. Access to mentoring and internal promotions can also lead to leadership, supervisory, and management roles.
Perm Drawbacks:
- Workplace politics: team dynamics with co-workers day and out, more opportunity for conflict depending on the facility type, size and teams.
- Less earning potential: compensation, compared to per diem and travel roles, may be lower.
- Burnout: Depending on the setting, repetitive work on a high-volume, day-to-day basis can eventually cause mental, emotional, and physical fatigue.
Per Diem Roles: PRN/As-Needed
Per diem jobs offer flexibility due to their “on-call” or “as-needed” scheduling nature. If you’re a healthcare professional in nursing, allied, or advanced practice, you can pick up or decline shifts based on your availability.
Per Diem Advantages:
- Flexible scheduling — picking and choosing when you work is ideal for individuals with other commitments, such as children, multiple jobs, or school, allowing them to select shifts based on their available schedule.
- Higher pay: per diem roles can sometimes pay 30–40% more than their staff counterparts.
- Variety: ample opportunities to work in different departments at multiple facilities.
- Networking opportunities: working in different settings allows you to observe how care is delivered differently based on the setting and also provides an opportunity to expand your professional network by meeting other professionals, experimenting with new environments, or enjoying some seasonal flexibility.
Per Diem Drawbacks:
- No guaranteed hours — per diem work does not always offer a reliable income, and it can be unpredictable.
- No employer benefits — no access to health benefit plans, personal paid time off, or retirement contributions.
- Less engagement — working with permanent teams and being the only outsider may lead to feeling left out.
- On-call expectations — not a lot of notice and last-minute scheduling may cause conflicts in your schedule
Travel roles: contract roles
Travel healthcare jobs are temporary assignments, often arranged through staffing agencies. Facilities rely on travel healthcare professionals to fill in during staffing shortages. Assignments in travel healthcare can run anywhere from 8 to 13 weeks, depending on the facility.
In addition to traditional travel roles, there are also local contracts – typically 13-week assignments based within a 50-mile radius of your tax home. While these positions do not include tax-free stipends, local contracts offer flexibility and the advantage of a full-time role with a pre-determined end date. This is a good way to try out roles at different facilities within your commute radius to see what suits you best.
Travel Advantages:
- Top-tier pay — weekly pay 30-80% back of staff level earnings, travel reimbursement, and sometimes a completion bonus.
- Tax-free stipends — housing, meals and incidentals (as a qualifying, true traveler).
- Resume-building — work in many of the nation’s top hospitals, city trauma centers, rural clinics, or underserved communities.
- Adventure and variety: explore a new city or state every 8-13 weeks – perfect for anyone who loves to see new places and likes change.
Travel Drawbacks:
- Frequent relocation — can be disruptive for some people and not ideal for families.
- Licensing hassle — requires compacts or state licensure and compliance needed for each new contract
- Limited benefits and job security — short assignments may or may not lead to extensions; not a lot of stability and usually no benefits like health insurance or 401k.
How to choose the best fit
Defining your priorities is the best place to start when considering what path to take in healthcare. For example, if you’re beginning your career, staff positions are great for learning and finding a mentor who can help guide you. Also, consider your lifestyle needs. If you need a job that lets you juggle family, school, or travel plans, then per diem might be a good fit for you. And don’t forget your financial goals. If making more money is your priority, travel jobs typically offer competitive compensation. On the other hand, per diem roles can be combined with perm and travel toles, which generate extra income. If benefits are a priority for you, staff positions provide steady income and benefits.
Here’s more to consider:
When thinking about which job type you’d like to focus on in healthcare, think about your experience and where you want to be. For example, staff or perm roles are perfect for training new healthcare providers. For travel and per diem jobs, you typically need at least 1-2 years of experience and some extra certifications under your belt.
Another factor is logistics and your location. Travel positions can be challenging because you’ll need licenses for different states and be prepared to relocate frequently. Per diem jobs are best suited for individuals who live in areas with a high concentration of hospitals or clinics to choose from. And staff roles usually mean you’re based in one place and plan on staying there for a while.
Visualizing the future
The benefit of the healthcare industry is that you’re not locked into just one path. As your life changes, your career can change with it. If you’re starting your career in a perm role and decide per diem will provide you more flexibility, you can move between perm and per diem with ease. Additionally, if you’re young and enjoy traveling with an open and flexible schedule, travel nursing, allied health, and locum tenens positions are an excellent choice.
With so many flexible options available, you can build a career that grows with you. Navigating your path requires successful planning and collaboration with industry experts, such as staffing and recruiting agencies, which can help you understand various roles. Working with a recruiter who understands your goals can help you stay proactive in managing licenses and certifications. The strategy of contracts and pay negotiations is the best way to achieve your desired outcomes. Let the experts at StaffDNA help you find a role in healthcare travel, staff, local, per diem, or locum tenens jobs today.

Calvin Hoye
Nursing
Check out these other great StaffDNA articles

When You Can See Everyone’s Pay
Imagine knowing exactly what you’ll earn before you apply for a job. No guessing and no wasting time on roles that can’t meet your financial needs.

Celebrating National CRNA Week 2026
Terminology changes quickly in healthcare, and there’s always an ever-growing column of information to understand.

Healthcare Staffing Trends That Will Shape 2026
Terminology changes quickly in healthcare, and there’s always an ever-growing column of information to understand.

If a Job Sounds Too Good to be True, It Probably Is
Terminology changes quickly in healthcare, and there’s always an ever-growing column of information to understand.

The Guide: Your Glossary of Healthcare Workforce Management Terms
Terminology changes quickly in healthcare, and there’s always an ever-growing column of information to understand.

IHS and Rural Healthcare Still Have Room for Hiring Optimism
Some of the biggest transformations in healthcare, specifically in nurse staffing