Fueling the Shift: Healthy Eating for Travel Nurses
A guide to eating well while working and traveling in healthcare
Being a travel nurse means you’re an essential worker, juggling work, family, friends, and the opportunity to travel to new places for your job. It’s a lot to manage. Maintaining a healthy lifestyle amidst all this—like figuring out where to fit in a balanced meal, a workout, and adequate sleep—poses an even bigger challenge. Starting with a balanced meal plan is crucial and a great way to ensure your routine for healthy living while on the go has a strong foundation.
Why is finding a way to nutritionally dense and healthy meals such a challenge? For many, the issue lies with time management. Busy healthcare workers working 12-hour shifts don’t have much time for meal planning and prep. Ordering takeout is easy and fast, and when you’re tired, cooking can feel like a chore. But it’s worth the effort. Eating home-cooked meals is associated with better quality, healthier food intake, and tends to be lower in fat, sodium, and sugar. It’s typically less expensive, too!
With a shift in perspective, a map of go-to food items, and an hour or two of food prep, meal plans are designed to keep you eating nutritionally all week.
The basic meal plan structure with hacks
While your job in healthcare demands a high level of attention to detail, meal planning doesn’t have to be as meticulous. Meal plans should focus on simplicity: making it easy to manage your meals without the stress of overthinking every detail. Each day of the week should consist of the following categories, which you can keep in mind when shopping for groceries:
Breakfast – A solid breakfast plan doesn’t have to be overly complicated to be enjoyable. Some quick-to-prepare options during a busy run in your facility include yogurt, a mixed fruit bowl, an egg and cheese quesadilla, or oatmeal in a cup. To kick off your day, choose healthy items that will provide the calories needed to get you through a long shift.
Lunch and Dinner – The key items to eat for lunch and dinner should consist of high-protein items like fish, poultry, or red meat. Alternatives if you’re vegan or vegetarian could be tofu, lentils or chickpeas. Some fun ideas to switch up the meals during the week: air-fried maple-glazed salmon, Chinese bourbon chicken, tofu tacos and sautéed Italian shrimp. And don’t forget the veggies. The average adult should aim for two to three servings of vegetables daily.
Snacks — Snacks should be nutritious and contain protein or fiber. They should have low calories but give you high energy without spiking your blood sugar. Items to consider would be fruit slices, Veggie straw chips, trail mix, and hummus, with celery and carrots on the side.
Mindful eating
Subconscious eating habits are real. Sometimes called mindless eating or stress eating, we often consume food without fully realizing our actions. Subconscious eating can significantly increase calorie intake—likely in the form of unhealthy snacks—and lead to weight gain. One of the best strategies is to keep nutritionally dense, low-calorie snacks on hand, so that when the urge to eat or nibble strikes, there’s a healthy option available.
Also, don’t “forget to eat.” Your body uses calories as fuel for everything you do, and in healthcare, that work can often be physically demanding. It’s estimated that 35% of nurses don’t take a meal break during their shift. Preparing and bringing meals or snacks with you during your shift ensures you have healthy, nutritious food readily available. Make sure you take the time to eat during your shift so you can maintain your energy levels.
Plan, prep and portion
Once you have a meal plan for the week, you can start planning your grocery list, planning when to cook, and prepping items in advance. When making a meal plan for the week, consider social engagements, planned dinners out, celebrations with food at work, and all the other circumstances that can affect your plan.
Remember that not every minute of every day has to be solely focused on perfectly balanced meals, and situations change. It’s okay to indulge and enjoy a donut for a snack or have a piece of cake at that retirement party, as long as the main focus of your week is on healthy and nutritious meals.
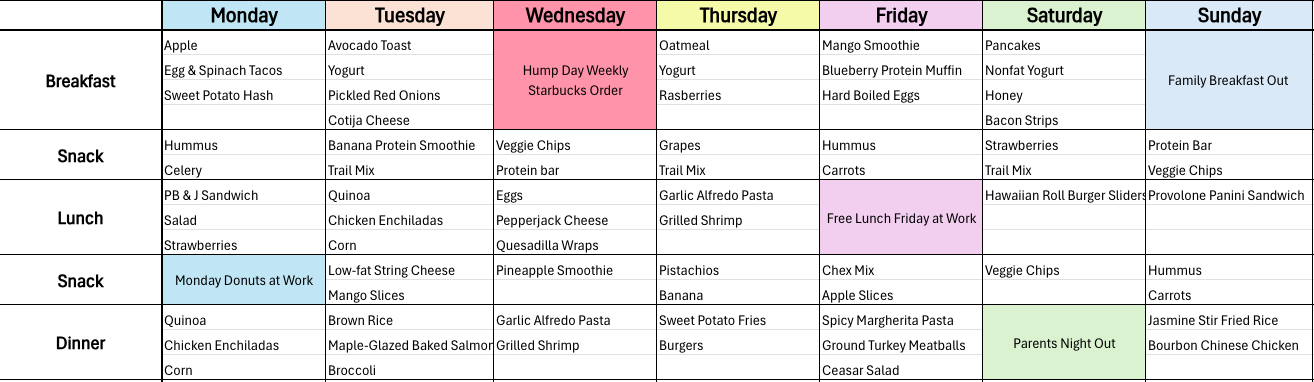
Here’s a sample meal plan that takes into account social events, workday treats and even a mid-week breakfast takeout:
Food for thought
Some tips to consider as you consider your meal planning journey:
- Meal prepping. Take an afternoon to pre-cook all your meals for the week and set them aside in the freezer for less cooking throughout the week.
- Prioritize sleep and water. Lack of sleep makes you 70% more likely to get into a workplace accident, and inadequate water intake makes you 25-50% less productive. That’s why sleep and water are so important.
- Cooking appliances. For days when you don’t have the energy, use quick cooking tools like an air fryer. Most proteins, like shrimp, salmon, chicken, or beef, take only 10 minutes to cook in an air fryer, depending on the portion size.
- Portions matter. Use a 1-cup measuring cup to divide a large trail mix bag into snack-size Ziplock baggies.
- Dinner tonight, lunch tomorrow. When cooking, make one extra plate. This eliminates the question of what to make for lunch the next day.
Nutrition is self-care too
Studies show that workers who maintained a poor and unbalanced diet were 66 percent more likely to report lower energy levels and productivity at work. A solid meal plan doesn’t just fuel your body—it supports your mind, sharpens your focus, and gives you the stamina to care for patients without sacrificing your health. For travel nurses, being intentional with food choices is one of the most impactful forms of self-care.
By meal prepping, choosing nutrient-rich snacks, and balancing your plate, you can thrive on any shift, in any state, at any time. Because when fueled right, you’re unstoppable. For more information about travel nursing, download the StaffDNA app and learn how two million healthcare professionals stay unstoppable in their careers.

Kelsey Moena
Sales
Check out these other great StaffDNA articles

Must-Have Gear for Healthcare Professionals: The Essential Items That Make Every Shift Better
Step into any hospital break room and you’ll observe something immediately: clinical professionals are always on the move. Nurses, doctors, radiology technicians, respiratory therapists, and so many others cover miles walking their shift, endure brutal 12-hour marathons, and juggle patient care with the physical demands of the job. When you’re this busy, having the right gear becomes necessary, not a luxury.

When You Can See Everyone’s Pay
Imagine knowing exactly what you’ll earn before you apply for a job. No guessing and no wasting time on roles that can’t meet your financial needs.

Celebrating National CRNA Week 2026
Terminology changes quickly in healthcare, and there’s always an ever-growing column of information to understand.

Healthcare Staffing Trends That Will Shape 2026
Terminology changes quickly in healthcare, and there’s always an ever-growing column of information to understand.

If a Job Sounds Too Good to be True, It Probably Is
Terminology changes quickly in healthcare, and there’s always an ever-growing column of information to understand.

The Guide: Your Glossary of Healthcare Workforce Management Terms
Terminology changes quickly in healthcare, and there’s always an ever-growing column of information to understand.